Unlocking the Power of Service Blueprints in Tech-Enabled Healthcare
A Practical Approach to Accelerating Product-Market Fit, Driving Cross-Functional Collaboration, and Blending Digital and Human Interactions
Imagine launching a tech-enabled healthcare startup where product-market fit is rapidly achieved, cross-functional teams collaborate effectively, and digital and human interactions are seamlessly integrated. While achieving this ideal state is an ongoing journey, one powerful tool can guide you in the right direction from the start: service blueprinting.
When I transitioned from digital therapeutics to healthcare delivery, I sought advice from industry veterans. One piece of wisdom consistently stood out: 'Start with a service blueprint.' While I had heard of service blueprints, I had little understanding of them. So, I set out on a mission to learn more.
In this article, I’ll share what I learned, including how service blueprints can accelerate product-market fit, drive cross-functional collaboration, and seamlessly integrate digital and human interactions. By the end, you'll understand why service blueprinting is an invaluable resource for any healthcare startup and the key steps to create your own.
What Is a Service Blueprint?
Service blueprinting is a technique that falls under the broader field of service design, which applies creative problem-solving and human-centered principles to improve service delivery and experiences.
As I delved into this technique, I discovered numerous approaches and frameworks. I found Practical Experience Blueprinting by Erika Flowers and Morgan Miller to be the most actionable for healthcare startups. In this section I'll outline the key steps of their approach, providing you with a roadmap to implement service blueprinting in your own healthcare startup. However, I strongly recommend reading their book (which is free to download) for a more comprehensive understanding. The depth and nuance provided in the full text offer invaluable insights that go far beyond what I cover here.
Step 1: Pick Your Scenario
A scenario is a defined pathway through a specific segment of the patient experience. For example, a scenario could be the process of a prospective patient booking and then attending their first provider encounter.
While there are many potential scenarios you could map, you should focus on the most common and critical interactions that will make up the majority of your service. You should always map out the primary success path (happy path) without any conditional branching, which is the ideal sequence of steps where everything goes as planned and the patient achieves their desired outcome. For example, this might include a new patient booking an appointment online, completing their intake forms, and attending the session.
Additionally, you might map out a secondary success path, which represents an alternative route that still leads to a successful outcome. For instance, a patient might call the office to book an appointment instead of using the online booking system.
Finally, you should also consider mapping out common problem paths in order to improve them. For example, if there are high patient no-show rates for the initial provider encounter, mapping out this scenario can help you identify the root causes and develop strategies to improve them.
Step 2: Map Out the Steps in the Scenario
Service blueprints are designed to depict the “surface-to-core” patient experience through a combination of steps and layers.
Steps represent the specific actions or interactions that directly affect the patient experience. These form the "surface" of the blueprint and might include activities such as booking an appointment, completing intake forms, or attending a consultation.
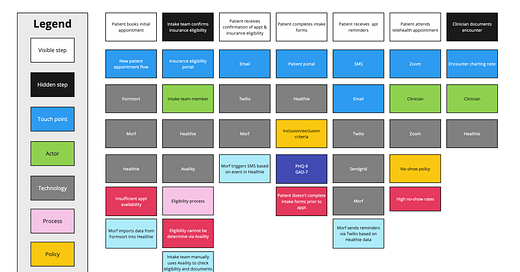
An important distinction within service blueprinting is between front-stage and back-stage activities. Front-stage activities are those that the patient directly experiences, such as interacting with a provider or booking an appointment. Back-stage activities are those that the patient doesn’t directly experience, such as a provider writing an encounter note or a billing department submitting an insurance claim. A service blueprint scenario marries the two together to show the linear path of both front-stage (visible) and back-stage (hidden) activities. In the diagram below you can see the front-stage steps (in white) and back-stage steps (in black) for an abridged scenario of a prospective new patient booking and attending their first appointment.

Step 3: Add in the Layers
Layers provide the underlying details that support and influence each step, forming the "core" of the blueprint. These layers add depth to your understanding of how each step is executed and what resources are involved. Not every step will necessarily involve all layers, but common layers include:
Touchpoints. These are the points of interaction between the patient and the business. E.g., a website, patient app or a video chat.
Actors. These are the roles of the people involved in the step (excluding the patient). For example, a therapist, physician, coach, or billing specialist. You would also list any third party actors involved, such as an external pharmacist.
Technology. These are the technology systems or infrastructure used in the step. For example, this might be your specific EHR (like Healthie), a form builder (like Formsort), or an integration platform (like Morf).
Policies. These are rules or guidelines that apply to the step. For example, your inclusion/exclusion criteria for accepting a new patient, payment policies, or dealing with any adverse events.
Measurements. We also added an additional layer for measures & assessments, since we have a heavy focus on measurement-based care. It was helpful to understand exactly which measures we expected to complete at various points in the program.
Below you can see the layers added to the steps, which now depict the full surface-to-core experience
The Strategic Advantages of Service Blueprinting for Healthcare Startups
Now that we've explored the components and creation process of a service blueprint, let's delve into why this tool is particularly valuable for early-stage healthcare delivery startups. By implementing service blueprinting, you can unlock several strategic advantages that will help your startup navigate the complex healthcare landscape more effectively.
Fostering Cross-Functional Collaboration
In tech-enabled healthcare, successful product development requires a symphony of expertise far beyond the traditional trio of product manager, engineer, and designer. You must incorporate ongoing input from diverse functional areas such as clinical, operations, finance, and regulatory, to name just a few.
Each functional area brings unique expertise and valuable insights to the table, approaching scenarios from their specialized point of view. For instance, the clinical team might prioritize treatment efficacy, operations may focus on scalability, and finance on cost-effectiveness. These diverse perspectives are essential for developing a comprehensive and effective healthcare solution. However, integrating these viewpoints can be challenging without a common framework. This is where service blueprints shine. They act as a universal language, allowing these diverse perspectives to align towards a common goal while preserving the value of each team member’s expertise.
In this way, your service blueprint becomes the ‘care delivery spec’ in the same way that a high-fidelity prototype might for a software product. It clarifies how everything works together, synthesizing insights from all functional areas. As a product leader, you can use this tool to listen to and incorporate various opinions, forming a clear path forward. The resulting blueprint can be referenced not only when building the service but also whenever there's a need to align understanding across teams later on.
Service blueprinting is also effective for facilitating conversations across both strategic and tactical levels. When building tech-enabled healthcare experiences, you must frequently transition from high-level strategic thinking to the nitty gritty details and back again. This framework allows you to easily do so. It’s also particularly useful for communicating the offering with executives or board members, who generally want the big picture, but sometimes want to dig into the details.
Seamlessly Blending Human and Digital Elements
In tech-enabled healthcare startups, the 'product' is not just a piece of software — instead, it’s a comprehensive service delivered primarily by healthcare providers. Beyond the ‘front stage’ patient-facing employees, there are also many people doing work behind the scenes. The role of technology in this context is to enhance the patient experience and drive operational efficiencies for the care team.
Service blueprints serve as a vital tool to bridge the gap between digital and human elements, providing a clear visualization of how technology impacts patients, staff, and third parties.
For example, consider the common challenge of verifying insurance eligibility during patient onboarding. Traditionally, this process involves manual verification by staff, which is time-consuming and frustrating for patients who are unable to quickly determine how much care will cost. Instead, a platform like Availity could be used to automatically check patient eligibility in real-time. Any ambiguous results could then be flagged for manual verification by the intake team. By doing so, startups can save staff time while providing real-time information to patients about their coverage.
By using service blueprints to map out the flow from automated checks to manual verification, teams can clearly see how these digital and human elements work together. This visual representation helps stakeholders understand the entire process, ensuring that all components are seamlessly integrated.
Accelerating Product-Market Fit Validation
For early-stage healthcare startups, maximizing runway while validating core assumptions is crucial. Service blueprints can play a pivotal role in this process, enabling founding teams to strategically allocate resources and avoid common pitfalls.
One such pitfall is the premature development of custom software. Many founding teams, eager to differentiate their offering, invest heavily in bespoke patient-facing apps or even EHR functionality. However, this approach often backfires. In conversations with industry leaders, a recurring theme emerged: regret over early investments in custom solutions that later proved unnecessary or misaligned with evolving clinical models.
A more effective strategy leverages service blueprints to identify the minimum viable tools needed to deliver and test your designed patient experience. This approach often involves a combination of manual processes (intentionally less scalable) and off-the-shelf, configurable solutions. By mapping out the end-to-end blueprint, you gain clarity on where technology is truly necessary to test core assumptions, allowing you to make informed decisions about tool selection and implementation.
In our experience at Noma, this blueprint-driven approach led us to a lean tech stack comprising a configurable EHR, form builder, and low-code automation platform. These versatile tools could be repurposed across various touchpoints in the patient journey, providing the flexibility needed to iterate rapidly based on real-world feedback.
This method not only conserves capital but also accelerates the validation of your riskiest assumptions. By focusing on delivering value through a well-designed service blueprint rather than prematurely investing in custom technology, you position your startup to achieve product-market fit more efficiently and effectively.
Navigating Common Pitfalls in Service Blueprinting
While service blueprints are powerful tools for healthcare startups, they come with their own set of challenges. Being aware of these potential pitfalls can help you maximize the effectiveness of your blueprinting efforts.
Balancing Detail and Usability
Service blueprints are designed to capture every interaction, touchpoint, and supporting process involved in delivering a service. This comprehensive nature can make them incredibly detailed and complex. While this level of detail is invaluable for identifying bottlenecks and opportunities for improvement, it can also render the blueprint impractical for everyday use by frontline staff or quick decision-making.
To address this challenge at Noma, we translate our service blueprints into practical standard operating procedures (SOPs) for specific functions. This approach maintains the strategic value of the comprehensive blueprint while providing actionable guidance for frontline staff and decision-makers. For example, we used the blueprint to create an SOP for the intake team to outline the key steps that must be taken when onboarding a new patient. Fun fact: try uploading your blueprint into ChatGPT and prompting it to create an SOP. It will require some finessing, but it does a surprisingly good job.
The Importance of Continuous Iteration
It's tempting to create an initial blueprint and consider the job done. However, the dynamic nature of healthcare delivery demands ongoing refinement. This iterative process involves regularly reviewing and updating the blueprint to reflect the current state of service delivery, incorporating feedback from frontline staff and patients, and identifying areas for improvement.
The Practical Experience Blueprinting methodology addresses this by distinguishing between two types of blueprints: current state and future state. Current-state blueprints focus on analyzing and improving existing processes, helping organizations understand how services are currently delivered and where inefficiencies lie. This type of blueprint is invaluable for identifying immediate opportunities for enhancement and ensuring that all team members have a shared understanding of the current service landscape. By contrast, future-state blueprints are ideal for envisioning zero-to-one services or significant overhauls of existing ones.
Blueprinting Your Path to Success
Service blueprinting has been one of the most influential and enlightening frameworks I've encountered as I transitioned into tech-enabled healthcare. I hope this article has provided you with valuable insights into how service blueprinting can positively impact your business and guide you in applying it effectively.
As you embark on your journey to integrate service blueprinting into your healthcare startup, remember that this framework is not just a one-time exercise but an ongoing process of refinement and optimization. By continuously iterating and adapting your blueprints, you can foster cross-functional collaboration, seamlessly blend human and digital elements, and accelerate your path to product-market fit.
Further reading
Blueprinting the Practical Way by Erika Flowers and Morgan Miller. This is the book that outlines the Practical Experience Blueprinting methodology
This is Service Design Doing by Marc Stickdorn et al . A seminal work on service design, offering a broader perspective on the discipline. Essential reading for those looking to deepen their understanding of service design principles and practices.
Mapping Experiences: A Complete Guide to Customer Alignment Through Journeys, Blueprints, and Diagrams by James Kalbach. This book offers a great overview of various journey mapping and blueprinting methodologies. It was the first book I read on the subject and led me to the Practical Experience Blueprinting methodology.
Design in Healthcare: Using Patient Journey Mapping from Delft University. This edX course provides a robust methodology for patient journey mapping. While not strictly required, it’s often helpful to start with a related methodology like patient journey mapping. A deep understanding of the patient experience is foundational for depicting the front-stage experience.
Thank you to Chipper Stotz, Dr. Andrea Auxier, and Dr Jeannette Waxmonsky for valuable input on drafts.
Thank you also to my incredible cross-functional teammates Dr Thomas Kim, Dr Jeannette Waxmonsky, Angela O'Conner, and Erin Scraper for their invaluable contributions and tireless efforts in bringing service blueprints to life at Noma. Your expertise, creativity, and collaborative spirit are instrumental in transforming our ideas into actionable strategies that continually enhance our patient experience and outcomes.



Fantastic overview and resource of a powerful service blueprint model that's new to me (this specific format, that is). Unfortunately, as I went to acquire more knowledge, I saw that Practical by Design has closed up shop, and all the links I can find on the Internet to the e-book and their Miro/Mural templates result in 404 errors. Fwiw, I've emailed the creators to let them know and see what might be done.... 🤞